- Spinal Injuries
- Hip Injuries
- Forefoot Injuries
- Knee Injuries
- Heel Injuries
- Midfoot / Arch Injuries
- Lower Leg Injuries - Calf & Soleus
- Upper Leg Injuries - Hamstring
- Medications
- Shoulder Injuries
- Ribcage / Chest Injuries
- Abdominal Injuries
- Head Injuries
- Elbow Injuries
- Hand Injuries
- Lower Leg Injuries - Achilles
- Ankle Injuries
- Upper Leg Injuries - Quadriceps
- Groin Injuries
- Lower Leg Injuries - Shin
- Spinal Injuries
- Hip Injuries
- Forefoot Injuries
- Knee Injuries
- Heel Injuries
- Midfoot / Arch Injuries
- Lower Leg Injuries - Calf & Soleus
- Upper Leg Injuries - Hamstring
- Medications
- Shoulder Injuries
- Ribcage / Chest Injuries
- Abdominal Injuries
- Head Injuries
- Elbow Injuries
- Hand Injuries
- Lower Leg Injuries - Achilles
- Ankle Injuries
- Upper Leg Injuries - Quadriceps
- Groin Injuries
- Lower Leg Injuries - Shin
 login
login

 View profile
View profile Add to friends
Add to friends Go to training log
Go to training log Go to race log
Go to race log Send a message
Send a message View album
View album
 CONNECT WITH FACEBOOK
CONNECT WITH FACEBOOK
Iliotibial Band Syndrome (ITBS) and ART Therapy
Do you have iliotibial band syndrome (ITBS)? Thinking about having Active Release Techniques (ART) done? This article will address ITBS and how ART can help.
Member Question from ering305
"Has anyone had ART done on their ITB? Did you find it effective? When/how long/what exactly did the ART specialist do to you?
After some research, I decided to go for it beginning last week. So far I've had four treatments over two weeks. I haven't felt a huge difference yet, and the specialist said it would take 8-10 treatments to break up the scar tissue effectively. On Runner's World I read that it takes 6-10 treatments as well. I also realize there is not a ton of research out there on the method."
Answer from Paul R. Krzesinski DC, ART®
 Iliotibial Band Function
Iliotibial Band Function
Member AMSSM
Thank you for your questions concerning ART® and its application with Iliotibial Band Syndrome (ITBS). I am a chiropractor and triathlete who uses ART® to help resolve repetitive-use injuries on a daily basis. In addition, I’ve personally dealt with ITBS in the past and understand how frustrating it can be (especially when it prevents you from a major competition).
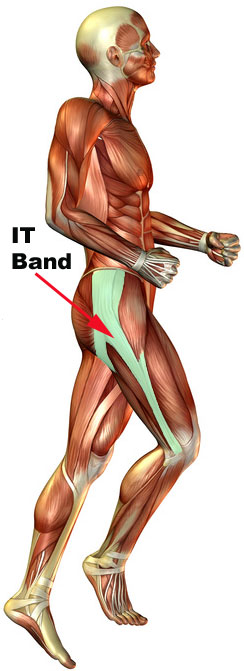
It is important to understand the function of the iliotibial band (ITB) as it relates to triathlon specific stressors and also how it can be affected by your day to day activities. It is impossible to discuss the ITB without looking first at the pelvic girdle. The ITB is a thick band of connective tissue that attaches at the top of the iliac crest and descends along the outside thigh to attach at the outside of knee (shown in green in the anatomical picture below). Its primary function is to assist with stabilizing the hip and knee particularly during single leg activities (walking, running, stepping, etc).
Classic Symptoms of ITBS
The classic symptoms of ITBS are noted as discomfort at the outside of the affected knee and a snapping or popping at the knee or the hip. Repetitive flexion and extension of the hip during running and cycling can cause the IT Band to snap back and forth over a bony prominence of the proximal lateral thigh called the greater trochanter. This ITB movement is one of the causes of “snapping hip syndrome”. In my clinical observations, I almost always find an involved IT-band with chronic knee problems, SI joint dysfunction, hip dysfunction or even foot problems.
Defining ART®
Active Release Techniques is a form of manual therapy that allows the practitioner to diagnose and treat soft-tissue injuries. Soft tissue refers to muscle, tendon, nerve and fascia which are often times injured with repetitive movements. The practitioner will apply a hand contact over the suspected involved tissue and perform specific movements to feel for changes in tissue texture, tension, movement and function. A typical treatment will involve 3-5 passes over the restricted tissue to mechanically break-up the adhesion. Application is applied to individual tolerances and has been described as a “hurt so good feeling” by many. ART® was developed by Michael Leahy DC in 1990 and has quickly evolved to become the gold standard in addressing soft tissue injuries.
ART® Treatment
As common as ITBS may seem in triathletes it is important to remember that not everyone responds the same to treatment nor is the cause of the symptoms always the same. A general exam including orthopedic testing, ROM, and functional movement screens (i.e. squat, lunge, step down test, etc) is a crucial first step in identifying the primary dysfunction and setting a road map of where to start treatment. Specific muscles tend to be chronically inflamed with ITBS and will be easily identified as tender to deep touch, thickened, and non-elastic resulting from the repetitive nature of the injury. These involved tissues including the quadriceps, ITB, hamstring, and TFL, usually respond quickly with ART®, a positive change being noted within 3-5 visits. Many times ART® treatment will also involve the hip flexors and pelvic stabilizers as these deeper, postural muscles tend to be a primary contributor to ITBS yet rarely are symptomatic.
Corrective exercises and stretching emphasizing normal muscle length, pelvic stability, and proper motor recruitment are all components of the rehabilitation process that will determine the success of ART® treatments and the prevention of future injury.
Case Study
Here is a link to a case study that does a relatively good job at outlining a classic rehabilitation program for a snapping hip syndrome incorporating ART®.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924651/?tool=pmcentrez
As athletes, we are all looking for that magic fix that will correct a problem so we can meet our training and racing goals- even if the problem has been chronic. ART® is arguably one of the best methods to correct soft tissue adhesions and when combined with a skilled therapist, very effective at correcting ITBS. However, individuals with core weakness will also need to perform strengthening exercises to complement ART® in order to ensure improvement and decrease the risk of recurrence.
If symptoms don’t improve after 6-10 visits than it’s time to try a different therapist.
For more information about ART® or to find a provider in your area please visit www.activerelease.com .
Paul R. Krzesinski DC, ART®
UNITED Chiropractic, Sports & Rehabilitation
Elkhorn, Wisconsin
Click on star to vote